Keratoconus Treatment at Lowest Cost
An affordable treatment for keratoconus by top ophthalmologist. Keratoconus surgery with advanced technologies.
Free Keratoconus Consultation
Get Keratoconus Estimate
Everybody Deserves To See The World Clearly.
We feel that everyone deserves to have a healthy vision. That’s why we’ve set out to deliver the finest eye care possible.
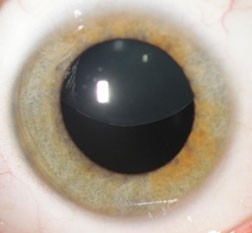
Common Characteristics of Keratoconus




Causes of Keratoconus
Genetics:
Keratoconus often has a genetic component, meaning it can run in families. Specific gene variations can lead to structural weaknesses in the cornea, increasing the risk of this condition.
Eye Rubbing:
Excessive and persistent eye rubbing can weaken the corneal tissue, potentially triggering or exacerbating keratoconus. Rubbing can create irregularities in the cornea’s shape over time.
Allergies and Eye Irritants:
Chronic exposure to allergens or eye irritants can lead to frequent eye rubbing and inflammation, contributing to the development or progression of keratoconus. Avoiding triggers is crucial.
Hear from our Patients

“After undergoing IPL treatment for dry eyes at EyeMantra, I’ve experienced a remarkable improvement in my eye comfort. The procedure was quick and painless, and the post-treatment care was excellent. My eyes feel refreshed, and I’m finally free from the constant irritation. Thank you, EyeMantra!”
– Neha
Frequently Asked Question's
Yes, treatments include artificial tears, prescription eye drops, lifestyle changes (e.g., using a humidifier), and in some cases, procedures like punctal plugs or IPL therapy.
Yes, untreated dry eyes can lead to corneal damage, infections, and discomfort. It’s important to seek treatment if you experience persistent dry eye symptoms.
Improvement can vary depending on the severity and cause of dry eyes. Some people experience relief within days, while others may take several weeks to notice significant improvement.
In severe cases, chronic dry eyes can lead to corneal damage and vision problems. Timely treatment and management can help prevent these complications.
