Get Best Treatment for Diabetic Retinopathy
Affordable Diabetic Retinopathy treatment by top eye doctors
Treatment for Diabeteic Eye Disease with advanced technologies
Online consultation on Diabetic Eye Disease
FREE Tele-Consultation
Book Appointment or Video Consultation online with top eye doctors
"*" indicates required fields
What is Diabetic Retinopathy?
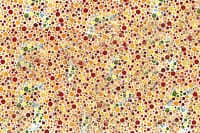
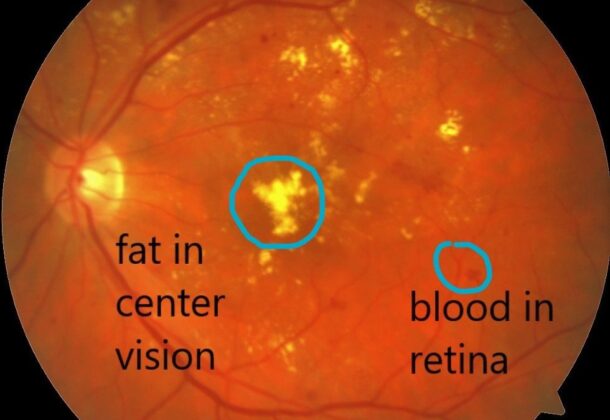
Diabetic retinopathy is one of those diabetic complications that affect the eyes. It’s caused by damage to the blood vessels present in the eyes, or more specifically, present in the retina of the eye.
In the primary stage, diabetic retinopathy may cause no signs or some signs of mild vision problems but can lead to severe conditions and make a person blind. Diabetic retinopathy can develop in anyone who has type 1 or type 2 diabetes. The longer you’ve got diabetes the less controlled your blood glucose is and the more likely you’re to develop this eye complication.
Symptoms of Diabetic Retinopathy
You might not have symptoms within the early stages of diabetic retinopathy. As the disease progresses, the symptoms appear even clearer. The symptoms are:





Diabetic retinopathy usually affects both eyes.
Diabetic Retinopathy Causes
Early occurrences. The longer you’ve got diabetes, the greater your risk of developing diabetic retinopathy:




Types Of Diabetic Retinopathy
There are two types of diabetic retinopathy, based on their intensity:
Early diabetic retinopathy:
Under this condition which is more commonly called non-proliferative diabetic retinopathy (NPDR), new blood vessels aren’t growing (proliferating).
When you have NPDR, the walls of the blood vessels in your retina start to weaken. Little bulges extend from the vessel walls of the smaller vessels, sometimes leaking fluid and blood into the retina.
Advanced diabetic retinopathy:
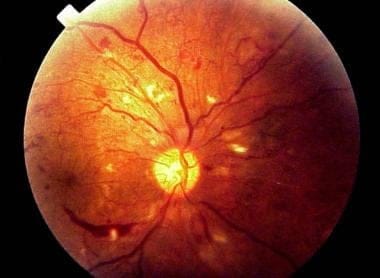
Diabetic retinopathy can reach this severe stage called proliferative diabetic retinopathy. And in this condition, damaged blood vessels close off, causing the expansion of the new, abnormal blood vessels within the retina, and may leak into the clear, jelly-like substance that fills the middle of your eye (vitreous).
Eventually, connective tissue stimulated by the expansion of the new blood vessels may cause the retina to detach from the rear of your eye. If the new blood vessels interfere with the traditional flow of fluid out of the attention, pressure may build up within the eyeball. This can damage the nerve that carries images from your eye to your brain (optic nerve), leading to glaucoma.
Stages of Diabetic Retinopathy
Diabetic retinopathy mostly affects both the eyes. The disease has three stages supported on which the treatment modalities are often discussed:

Diabetic Retinopathy Risks
Diabetic retinopathy involves the abnormal growth of blood vessels within the retina. Complications can lead to serious vision problems:
Vitreous hemorrhage
The new blood vessels may bleed into the clear, jelly-like substance that fills the centre of your eye. If the amount of bleeding is small, you might see only a few dark spots (floaters). In severe cases, blood can collect in the vitreous cavity and block your vision.
Vitreous hemorrhage alone cannot cause total vision loss. The blood often clears from the attention within a couple of weeks or months. Unless your retina is broken, your vision may return to its previous clarity.
Retinal detachment
The abnormal blood vessels related to diabetic retinopathy stimulate the expansion of connective tissue, which may pull the retina far away from the rear of the attention. This may cause spots floating in your vision, flashes of sunshine, or severe vision loss.
Glaucoma
New blood vessels may grow within the front part of your eye and interfere with the traditional flow of fluid out of the attention, causing pressure within the eye to build up which may damage the optic nerve.
Blindness
Eventually, diabetic retinopathy, glaucoma or both can cause complete vision loss.
Diabetic Retinopathy Treatment
Treatment depends largely on the sort of diabetic retinopathy you’ve got and the way it’s severe is geared to slowing or stopping the progression of the condition.
Early Diabetic Retinopathy Treatment
If you’ve got mild or moderate non-proliferative diabetic retinopathy, you’ll not need treatment directly. However, your ophthalmologist will closely monitor your eyes to work out once you might need treatment.
Work together with your diabetes doctor (endocrinologist) to work out if there are ways to enhance your diabetes management. When diabetic retinopathy is mild or moderate, good blood glucose control can usually slow the progression.
Advanced Diabetic Retinopathy Treatment
If you’ve got proliferative diabetic retinopathy or macular edema, you will need prompt surgery. Depending on the precise problems together with your retina, options may include:
- Photocoagulation / Retinal Laser – This laser treatment, also referred to as focal laser treatment, can stop or slow the leakage of blood and fluid within the eye. During the surgery, leaks from abnormal blood vessels are treated using laser burns. If you had blurred vision from macular edema before surgery, the treatment won’t return your vision to normal, but it’s likely to scale back the prospect the macular edema may worsen.
- Panretinal photocoagulation/ Retinal Laser – This laser treatment, also referred to as scatter laser treatment, can shrink the abnormal blood vessels. During the procedure, the areas of the retina far away from the macula are treated with scattered laser burns. The burns cause the abnormal new blood vessels to shrink and injure them. Your vision is going to be blurry for a few days after the procedure. Some loss of sight or night-sight after the procedure is feasible.
- Vitrectomy – This procedure uses a small incision in your eye to get rid of blood from the centre of the attention (vitreous) also as the connective tissue that’s tugging on the retina.
- Eye injections – These medications, called vascular endothelial protein (VEGF) inhibitors, may help stop the growth of the latest blood vessels by blocking the consequences of growth signals the body sends to get new blood vessels. Your doctor may recommend these medications, also called anti-VEGF therapy, as a stand-alone treatment or together with pan-retinal photocoagulation.
Surgery or Injection often slows or stops the progression of diabetic retinopathy, but it isn’t a cure. Because diabetes may be a lifelong condition, future retinal damage and vision loss are still possible.
Prevention From Diabetic Retinopathy
You can’t always prevent diabetic retinopathy. However, regular eye exams, good control of your blood glucose levels, and early intervention for vision problems can help prevent severe vision loss.
If you’ve got diabetes, reduce your risk of getting diabetic retinopathy by doing the following:
Manage your diabetes
Make healthy eating and physical activity a part of your daily routine. Try to get a minimum of 150 minutes of moderate aerobic activity, like walking, each week. Take oral diabetes medications or insulin as directed by your doctors.
Monitor your blood sugar level
You may get to check and record your blood glucose level several times each day — more frequent measurements could also be required if you’re ill or under stress. Ask your doctor how often you need to test your blood sugar.
Ask your doctor about a glycosylated hemoglobin test
The glycosylated hemoglobin test, or hemoglobin A1C test reflects your average blood sugar level for the two-to-three month period before the test. For most people, the A1C goal is to be under 7 percent.
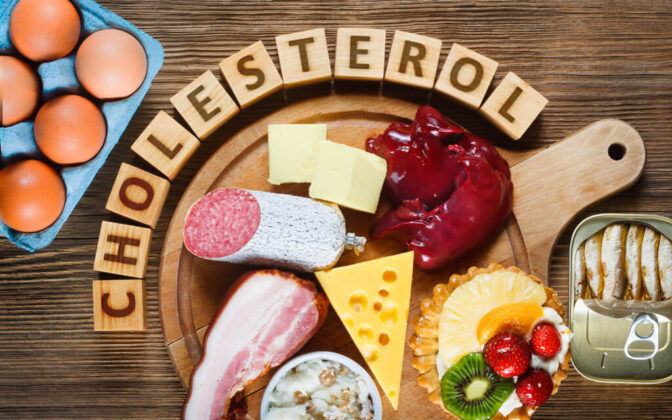
Keep your blood pressure and cholesterol under control
Opting for a healthy diet and regular exercise will be beneficial. Sometimes medication is needed too.
If you smoke or use other types of tobacco, ask your doctor to help you quit
Smoking increases your risk of many kinds of diabetes complications, including diabetic retinopathy.
Pay attention to vision changes. Contact your ophthalmologist directly if you experience sudden vision changes or your vision becomes weak.
Diabetic Retinopathy treatment Cost
The complete cost of Diabetic Retinopathy treatment depends upon the “type of procedure” that you go through. The cost of treatment varies between Rs.3,000 to Rs.50,000. Below are estimated cost of some of the procedure, injections, testing and surgery involved in treatment of Diabetic Retinopathy
| Diabetic Retinopathy Treatment | Cost (₹) |
|---|---|
| Fundus Angiography | 2,500 |
| OCT | 2000-3000 |
| Yag Laser (Single eyes) | 2000 – 3000 |
| Green Laser (Single Eye) | 2000 – 3000 |
| YAG iridotomy | 2000 – 3000 |
| Injection Avastin | 10000 – 15000 |
| Injection Razumab | 20000 – 25000 |
| Injection Accentrix | 30000 – 40000 |
| Retinal Detachment Surgery | 40000 – 45000 |
| Vitrectomy | 30000 – 40000 |
We also provide charitable retina treatment services to the “underprivileged sections of society”. So if you need retinal eye treatment, but are unable to afford the treatment expenses, you can come to our hospital and his entire treatment will be done “free of cost or at a very nominal price”.
Best Eye Hospitals for Diabetic Retinopathy treatment
India has one of the best eye hospitals for cataract surgery such as AIIMS, Sankara Nethralaya, LVPEI and Eye Mantra. Eye Mantra is one of the leaders in Diabetic Retinopathy treatment with over 1,000+ eyes operated so far by its doctors.
At Eye Mantra, we offer the best diabetic retinopathy treatment in India. Our wide range of services includes retina care with retinal detachment treatment and diabetic retinopathy management, based on laser and other surgical procedures at an affordable cost in Delhi-NCR.
Our experienced diabetic retinopathy specialists conduct a comprehensive eye examination to detect and assess the severity of the disease through extensive tests. The treatment is based on factors like stage of the disease, age of the patient, and consultations of the retina specialist.
Diabetic Retinopathy Facilities









FAQ's
Diabetic retinopathy is one of those diabetic complications that affect the eyes. It’s caused by damage to the blood vessels present in the eyes, or more specifically, present in the retina of the eye.
There are two types of diabetic retinopathy, based on their intensity:
- Early diabetic retinopathy
Advanced diabetic retinopathy
Some of the preventive measures include:
- Managing blood sugar levels
- Glycosylated Hemoglobin test
- Regular eye examination
- Control on cholesterol and blood pressure levels
If you constantly monitor your blood sugar levels and have your diabetes in control. The chances of you getting affected from diabetic retinopathy decrease. But at the same time, maintain the blood pressure and cholesterol levels.
A patient suffering from diabetic retinopathy can seek help from Dr. Shweta at Eye Mantra . Because when it comes to diabetic retinopathy, the patient would require help from both, a diabetologist and ophthalmologist as well. The medical doctors or the diabetologist will help you regulate your blood sugar levels. And the ophthalmologist will examine the eye issues.Eye Mantra provides the best treatment for diabetic retinopathy.
It is one of the complications of diabetes which even gets worse with time, if not treated. And yes, in some unfortunate cases, people have gone blind if they have not taken action against the disease at a proper time.
There is no certain time frame. It depends upon your blood sugar management. Even a 25 years old can go blind because of diabetic retinopathy whereas a 90 years old man can have the least vision issues if he controls his blood sugar levels.
There is no specified surgical treatment for resolving Diabetic retinopathy permanently. But, if you get the appropriate treatment in time, you can definitely prevent yourself from vision loss, or reduce its effect.
The two best treatments as prescribed by the doctors are:
Laser treatment, to treat the weakened blood vessels in the eye and growth of the new ones. It also helps in stabilizing some cases of maculopathy.
Another one is eye injections to treat maculopathy to prevent further destruction of the eye.
In most cases, yes it is. But there are certain ways in which you can prevent or delay blindness. Try to get timely treatment and surgeries as your doctors say after the examination of your case.
Careful management of your diabetes is the best way to prevent vision loss. If you’ve got diabetes, see your ophthalmologist for a yearly eye exam with dilation. Pregnancy may worsen diabetic retinopathy, so if you’re pregnant, your ophthalmologist may recommend additional eye exams throughout your pregnancy.
Contact your ophthalmologist directly if your vision changes suddenly or becomes blurry, spotty, or hazy.
There are multiple good retina doctors in India. Eye Mantra has some of the top Diabetic retinopathy doctors / surgeons. Dr. Shweta Jain is one of the best Diabetic retinopathy specialists in India. Dr. Shweta Jain has successfully performed more than 1000+ Diabetic retinopathy treatments so far. The results from the Eye Mantra Diabetic retinopathy surgery program turns out to be better for many people. Post Diabetic retinopathy surgery, Improved vision and depth perception.