Best Uveitis Treatment by top eye doctors
- Affordable and reliable Uveitis Surgery by top doctors
- Interactive consultation available with 24/7 eye care facilities
- Pre and post video consultation online with top eye doctors
FREE Tele-Consultation
Book Appointment or Video Consultation online with top eye doctors
"*" indicates required fields
WHAT IS UVEITIS?
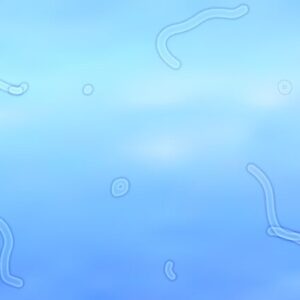
Uveitis is a form of eye inflammation. It affects the middle layer of tissue in the eyewall (uvea), and its warning signs come suddenly. The uvea involves the center layer of pigmented structures of the eye and incorporates the iris, ciliary body, and choroid. Uveitis is a dangerous disease and requires immediate assessment and treatment by an ophthalmologist It is frequently connected with other visual issues.
Types of Uveitis
Uveitis is usually classified by where it occurs in the eye.
Anterior Uveitis
It occurs in the front of the eye. It is the most common form of uveitis, frequently occurring in young and middle-aged people. Many cases occur in healthy people and may only affect one eye but some are associated with rheumatologic, skin, gastrointestinal, lung, and infectious diseases.
Intermediate Uveitis
It is commonly seen in young adults. The center of the inflammation often appears in the vitreous. It has been linked to several disorders including, sarcoidosis and multiple sclerosis.
Posterior Uveitis
It’s a term used when all three major parts of the eye are affected by inflammation. Behcet’s disease is one of the most well-known forms of panuveitis and it greatly damages the retina. Intermediate, posterior, and panuveitis are the most severe and highly recurrent forms of uveitis. They often cause blindness if left untreated.Intermediate, posterior, and panuveitis are the most severe and highly recurrent forms of uveitis. They often cause blindness if left untreated.
Symptoms of Uveitis
Symptoms may occur suddenly and get worse quickly, though in some cases, they develop gradually. They may affect one or both eyes. Occasionally, there are no symptoms, and signs of uveitis are observed on a routine eye exam.
Some of the signs and symptoms of uveitis may include:





Causes Of Uveitis
The cause for uveitis is frequently unknown. It can be some of the time related to another ailment or disease from an infection or microscopic organisms. An immune system illness happens when your immune system attacks a part of your body.
Immune system conditions
- Rheumatoid arthritis
- Psoriasis
- Arthritis
- Ulcerative colitis
- Kawasaki infection
- Crohn’s infection
- Sarcoidosis
Infections
- AIDS
- Herpes
- CMV retinitis
- West Nile infection
- Syphilis
- Toxoplasmosis
- Tuberculosis
Other expected reasons
- Exposure to a toxin that enters the eye
- Bruising
- Injury
- Trauma
Uveitis Diagnosis
Following are some of the tests that should be included for diagnosing Uveitis:
- An eye chart or visual acuity test,
- A funduscopic exam,
- An ocular pressure test,
- A slit lamp exam.
Treatment Of Uveitis
Treatment relies upon the cause and the type of eye that is infected.
Some recommended medicines for the treatment of uveitis are:
Steroid Medication
Most instances of uveitis can be treated with steroid medication. A medication called prednisolone is normally utilized. Steroids work by disturbing the typical capacity of the immune system so they no longer deliver the chemicals that irritate. Steroid medications come in various structures, and the sort utilized will frequently rely upon the regions of your eye affected by uveitis.
Steroid Eye Drops
They are typically the primary treatment utilized for uveitis that influences the front of the eye and isn’t caused by any disease. Contingent upon your symptoms, the prescribed portion can go from utilizing eye drops each hour to regular intervals. You may get a temporary blurred vision after utilizing the drops. It is prompted not to work until your vision gets back to normal.
Try not to quit utilizing your eye drops until your ophthalmologist tells you. Ensure the treatment goes on until the infection has been completely treated. Else, it may come back again and this time symptoms may be more awful than the past one.
Depending on your symptoms, the recommended dose can range from having to use eye drops every hour to once every 2 days.
You may have temporary blurred vision after using the drops. Do not drive or operate machinery until your vision returns to normal.
In some people, steroid eye drops can increase pressure in the eye. The eye specialist (ophthalmologist) will check for this and advise you if this happens.
Steroid Infusions
If the center or back of your eye is affected or steroid eye drops have not worked, you may require steroid infusions. Anaesthetic eye drops are utilized to numb your eye so you won’t feel any pain or uneasiness.
Steroid infusions generally don’t cause any results, yet at times the weight in the eye increments after utilizing the infusion. The ophthalmologist will check for this and will advise you if this occurs.
Steroids Tablets Or Capsules
Steroids tablets or capsules are the strongest types of steroids. They’re normally utilized if steroid eye drops and infusions have not worked or are unsuitable, or for uveitis affecting the rear of the eye. What amount of time you’ll need to require for steroid tablets relies upon how well you react to treatment and whether you have an underlying immune system condition.
Short-term results of steroids tablets or capsules can incorporate weight increase, expanded craving, a sleeping disorder, and mood changes, for example, feeling irritable or restless. In the long term, they can cause osteoporosis, thinning of the skin, and an increased danger of disease. To decrease the odds of any results, you will be prescribed a less possible dose that will control your symptoms.
Mydriatic Eye Drops
If you have uveitis that affects the front of your eye (anterior uveitis), you may be given mydriatic eye drops as well as steroid medicine.
These eye drops enlarge (dilate) your pupils and relieve pain by relaxing the muscles in your eye. They can also reduce your risk of developing glaucoma, which affects vision.
However, mydriatic eye drops can cause some temporary blurring of your vision and problems focusing on your eyes.
Surgical Option For Uveitis
Vitrectomy Surgery
Vitrectomy is a surgical technique in which the vitreous humor several procedures, including scar tissue removal, laser retinal detachment repair, and macular hole treatment. To help keep the retina in place after surgery, saline, a gas bubble, or silicone oil can be injected into the vitreous gel.
A vitrectomy includes tenderly sucking out the jam-like substance that fills within the eye (glassy humor gel). It tends to be finished utilizing either an overall sedative or a neighborhood sedative.
It’s usually only recommended if you have repeated or severe uveitis, or if the situation is caused by infections. During the operation, the fluid inside your eye will be temporarily replaced with either a bubble of air or gas (or a mixture of the 2) or a liquid substitute. Eventually, the vitreous humor will naturally replace itself.
Risks Factors of Vitrectomy
Like all operations, a vitrectomy carries a risk of complications. These includes:
- Infection
- Bleeding
- Detached retina
- Poor vision
- Glaucoma
- Cataract in the eye
Uveitis After Care Measures
During the surgery, you will be feeling very drowsy as you will be given some medicines to numb your eye and also relax you. Post the operation, it is advisable to rest for at least a minimum period of 7 days. Doctors advise not to participate in any of the following activities:
- Driving
- Reading
- Bending Over
- Lifting anything heavy for 4 weeks
- Avoid Splashing or putting water in the eyes
- Contact Lenses might not fit properly
Uveitis Facilities









FAQ's
Patients may experience pain when the pupil contracts, which occurs when light strikes the iris if the iris is inflamed. White blood cells and protein in the eye fluid can be observed under a microscope if uveitis is present. Blood tests and x-rays may be recommended by the doctor.
Uveitis can damage the eyes permanently, resulting in an irreversible visual loss. Uveitis can also be caused by another disease or condition, if not treated, which might result in significant illness.
This is usually a severe discomfort. Uveitis pain can strike quickly or develop gradually, with little pain but gradually blurring of vision. Other uveitis symptoms include burning.
A complete examination by an ophthalmologist is required to diagnose uveitis, which includes a careful look at your previous and present health history. Doctors perform tests like an eye chart or visual acuity test, a funduscopic exam, an ocular pressure test, and a slit lamp exam for diagnosing uveitis.
On your first visit you will be examined for refraction, intraocular pressure check, vision, slit-lamp, and dilated retinal examination. Other than this doctor consultation, scans if required, advice on laser or surgery, and medical prescriptions as per the requirement.
Yes, your eyes will be dilated at every visit if you have problems in the posterior segment of the eye, such as uveitis, or if you have systemic problems that are affecting the retina because of diabetes or hypertension. Another reason can be the symptoms that point to retinal or optic nerve involvement.
Uveitis refers to a variety of intraocular inflammatory disorders and is an auto-immune disease of the eye.
There are at least two possible direct interactions between stress and uveitis: stress could be a risk factor for uveitis, or it could be a reaction to the symptoms and limits imposed by uveitis, such as decreased visual acuity.