Facing diabetes isn’t just about managing blood sugar levels—it’s also about keeping an eye on… well, your eyes! Diabetic retinopathy is a common sidekick of diabetes, and it can lead to some serious vision issues if it’s not caught and treated early.
In this blog, we’ll unpack everything you need to know about this eye condition. We’ll walk through the different stages, what signs to look out for, and the treatments that can help keep your vision clear. So, let’s jump in and learn how to stay one step ahead of diabetic retinopathy!
Contents
What is Diabetic Retinopathy?
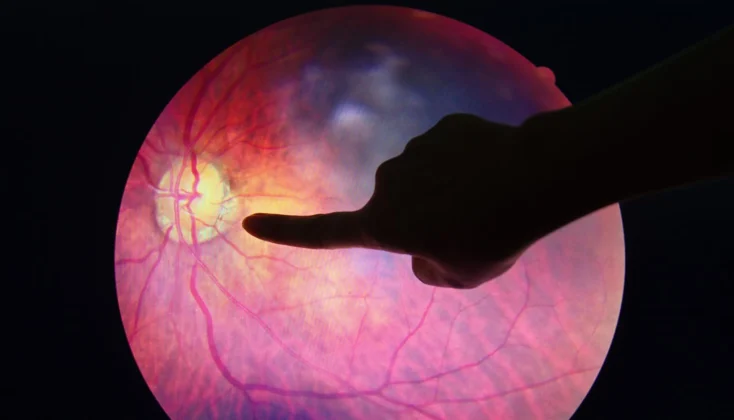
 Diabetic retinopathy is a condition that can develop in people with diabetes, particularly when high blood sugar levels persist over time. It affects the retina, which is the light-sensitive layer at the back of the eye essential for clear vision. When blood sugar levels are consistently high, it can damage the tiny blood vessels that nourish the retina. This damage can lead to a range of problems.
Diabetic retinopathy is a condition that can develop in people with diabetes, particularly when high blood sugar levels persist over time. It affects the retina, which is the light-sensitive layer at the back of the eye essential for clear vision. When blood sugar levels are consistently high, it can damage the tiny blood vessels that nourish the retina. This damage can lead to a range of problems.
- These tiny vessels can swell and weaken, leading to leaks of blood and fluid into the retina.
- Alternatively, they can become so damaged that they close off, preventing adequate blood flow, which can cause new, abnormal blood vessels to grow.
- Both scenarios are harmful to eye health and can compromise vision.
Prolonged damage to these vessels due to high blood sugar is a gradual process, meaning symptoms might not be noticeable until the condition has advanced, making regular eye check-ups crucial.
The Stages of Diabetic Retinopathy
Diabetic retinopathy doesn’t just show up overnight; it develops in stages, each one more serious than the last. Understanding these stages can help catch the condition early and prevent vision loss. Here’s how it progresses:
Early Diabetic Retinopathy
 This is also called non-proliferative diabetic retinopathy (NPDR). This is the earliest stage where small areas in the blood vessels of the retina, called microaneurysms, start to balloon and form. At this stage, changes are minimal and may not affect your sight.
This is also called non-proliferative diabetic retinopathy (NPDR). This is the earliest stage where small areas in the blood vessels of the retina, called microaneurysms, start to balloon and form. At this stage, changes are minimal and may not affect your sight.
- Moderate NPDR
Moving a step up, the blood vessels that nourish the retina are now affected more extensively. They can change in diameter, and more of them become blocked. This stage can lead to changes in blood flow and the health of the retina, potentially impacting your vision. - Severe NPDR
At this point, the blood vessel blockages cause a significant decrease in blood flow to the retina. The body responds by sending signals for new blood vessels to grow.
Advanced Diabetic Retinopathy
This is the most advanced stage and is also known as proliferative diabetic retinopathy. The signals sent previously trigger the growth of new blood vessels. But there’s a problem — these new vessels are weak and can leak blood, leading to serious vision problems, including the possibility of blindness.
Early Warning Signs and Symptoms

When diabetic retinopathy begins to creep in, it can bring along some telltale signs. However, in its early stages, you might not notice anything is wrong. As it progresses, here are some symptoms to watch for:
- Your vision might start to blur, making it hard to see details, read, or drive.
- These are small spots or lines that float across your vision, usually noticeable against a bright background like a clear sky or a white computer screen.
- Finding it hard to see when the lights go down? This could be a sign of diabetic retinopathy.
- You might notice patches where your vision is hazy or completely gone.
- In advanced stages, diabetic retinopathy can lead to significant vision loss or even blindness.
It’s worth noting that these symptoms can come and go, or they may progressively worsen. Don’t wait for symptoms to become severe before seeking help. Catching diabetic retinopathy early can help prevent irreversible damage to your eyesight.
That’s why regular eye exams are so critical, especially if you have diabetes. Your eye doctor can spot the early signs of retinopathy, often before you notice any changes in your vision. So, if you’re experiencing any of these symptoms or if you’re due for a check-up, don’t delay.
Risk Factors for Diabetic Retinopathy
While having diabetes is the primary risk factor for developing diabetic retinopathy, not everyone with diabetes will experience this eye condition. Certain factors can elevate your risk, making it crucial to be aware and proactive in managing your health. Here are the key risk factors for diabetic retinopathy:
- The longer you’ve had diabetes, the greater your risk of developing diabetic retinopathy. After 20 years of living with diabetes, nearly all patients with type 1 diabetes and more than 60% of patients with type 2 diabetes have some degree of retinopathy.
- High blood sugar levels can damage the blood vessels in the retina over time, leading to retinopathy.
- High blood pressure is another risk factor for diabetic retinopathy.
- High levels of cholesterol can contribute to the blood vessel damage that leads to diabetic retinopathy.
- Women with diabetes who become pregnant face a higher risk of developing diabetic retinopathy.
- Smoking or using other forms of tobacco can increase your risk of diabetic retinopathy, as well as other diabetes complications.
Complications of Diabetic Retinopathy
 The complications associated with diabetic retinopathy can lead to various vision problems like:
The complications associated with diabetic retinopathy can lead to various vision problems like:
- Vitreous hemorrhage – The abnormal growth of new blood vessels in the retina part of the eye causes fluid release into the vitreous chamber. As the chamber gets filled with the fluid, there is the appearance of dark floaters in vision, leading to complete blocking of vision. If detected early it can be prevented by removing the fluid and the vision can be restored to normal until and unless the retina gets damaged.
- Retinal detachment – In this, as the disease progresses and the diabetic retinopathy stimulates the growth of the scar tissue, it causes the retina to detach from the back of the eye. This causes spots floating in the vision, flashes of light, and causes severe vision loss.
- Glaucoma – There is an increase in the formation of new blood vessels in the front part of the eye which blocks the flow of fluid into the eye and causes increases in the pressure of the eye leading to glaucoma. Diabetic retinopathy also damages the optic nerve.
Diagnosing Diabetic Retinopathy
 If you have diabetes, regular eye exams are crucial, even if your vision seems fine. Here are the primary tests used to diagnose diabetic retinopathy:
If you have diabetes, regular eye exams are crucial, even if your vision seems fine. Here are the primary tests used to diagnose diabetic retinopathy:
- A comprehensive eye exam where your eye doctor will ask about your medical history and any vision problems you’re experiencing.
- Visual acuity testing checks how well you see at various distances.
- During the dilated eye exam, drops are placed in your eyes to widen the pupils, allowing the doctor to examine the retina and optic nerve for signs of damage.
- If your doctor suspects retinopathy, they might recommend fluorescein angiography. In this test, a special dye is injected into your arm, and pictures are taken as the dye circulates through your eye’s blood vessels.
- OCT is like an ultrasound for your eye, but it uses light instead of sound waves to capture highly detailed images of the retina. It can show the thickness of the retina, which helps in identifying swelling, fluid accumulation, or changes in the retina’s structure.
These tests can help your doctor detect diabetic retinopathy in its earliest stages, even before you notice any vision problems.
Can Retinopathy Be Cured?
Currently, there is no outright cure for retinopathy, including diabetic retinopathy. The damage to the retina caused by this condition is often irreversible. However, early detection and treatment can significantly slow its progression, reduce the risk of vision loss, and in some cases, improve vision.
While diabetic retinopathy is a common complication of diabetes, taking proactive steps can significantly reduce your risk of developing this eye condition or slow its progression if you already have it. Here’s how you can protect your vision:
- Keeping your blood sugar levels within your target range is the cornerstone of diabetic retinopathy prevention.
- Maintaining blood pressure and cholesterol within recommended levels helps protect your eyes and reduces the risk of other diabetes complications.
- A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support overall health and help manage diabetes.
- Regular physical activity also plays a key role in controlling blood sugar levels.
- Quit Smoking and limit Alcohol Consumption
- Regular check-ups with your endocrinologist or primary care provider are essential
Conclusion
In conclusion, whether you’re navigating the challenges of eye health as a person with diabetes or you’re specifically tackling the complexities of diabetic retinopathy, there’s hope and help available.
If you’re noticing changes in your vision, experiencing symptoms related to the retina, or simply looking for expert guidance on managing diabetic retinopathy, Retina Surgery at EyeMantra is here to support you. Book your free appointment now at +91 9711116605 and take the first step towards a clear vision.
For those determined to tackle diabetes head-on and explore ways to manage and possibly reverse its effects through lifestyle changes, At MantraCare, our online diabetes treatment program offers a comprehensive approach.
With personalized diet plans, exercise routines, yoga sessions, and continuous support from our dieticians and health coaches, you have a community ready to help you make meaningful changes. So, join our program and start your journey towards a healthier life, aiming to reduce or reverse the impact of diabetes naturally.

 This treatment is used to seal or shrink leaking blood vessels in the retina, slowing the leakage of fluid and reducing the amount of fluid in the retina. It’s often recommended for people with macular edema (swelling of the central retina) or proliferative diabetic retinopathy (PDR). The laser can also destroy abnormal blood vessels that form in PDR.
This treatment is used to seal or shrink leaking blood vessels in the retina, slowing the leakage of fluid and reducing the amount of fluid in the retina. It’s often recommended for people with macular edema (swelling of the central retina) or proliferative diabetic retinopathy (PDR). The laser can also destroy abnormal blood vessels that form in PDR. This surgical procedure is typically reserved for advanced proliferative diabetic retinopathy. During a vitrectomy, the vitreous gel, along with any blood and scar tissue that’s causing problems in the retina, is removed from the eye. This helps clear the path for light to reach the retina and can prevent
This surgical procedure is typically reserved for advanced proliferative diabetic retinopathy. During a vitrectomy, the vitreous gel, along with any blood and scar tissue that’s causing problems in the retina, is removed from the eye. This helps clear the path for light to reach the retina and can prevent 
