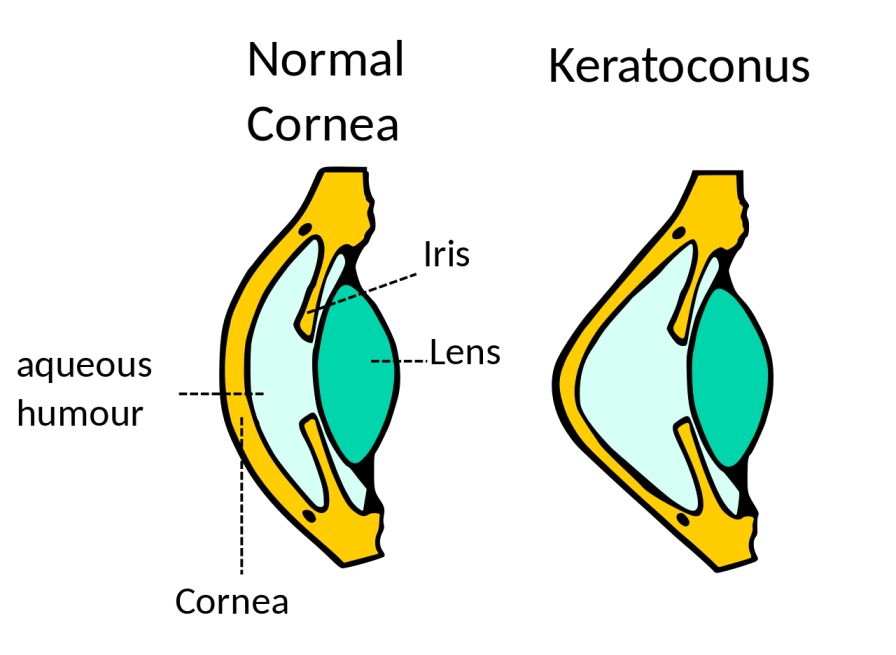
In our eye, there is a presence of an outer protective covering called the cornea. The cornea is the transparent dome-shaped covering of the eye. It helps in focusing the light and also assists in the formation of the vision. There are small collagen fibres present in the eye which help in maintaining the shape of the cornea. As the collagen fibres weaken due to the absence or presence of low amounts of antioxidants, they then lose their ability to hold the cornea in proper shape. This causes the cornea to bulge out and form a cone-like structure.
Contents
What Is Keratoconus?
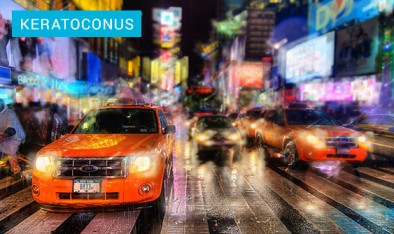
When the cornea turns into a shape of a cone then this eye condition is termed keratoconus. It is not a very common eye condition. If a person suffers from keratoconus then they have blurred vision and have difficulty in viewing objects. This is because the cone-shaped cornea does not help in focusing the light and hinders the image formation causing blurry vision.
Changes in the shape of the cornea cause change in the vision and you may not be able to see clearly without the help of eyeglasses. Keratoconus is generally mistaken as a normal eye condition (near-sightedness or far-sightedness) as you may feel at ease while using an eyeglass. Though for some people the condition may not be as serious and can be cured easily for some it may require to get corneal transplantation for proper vision.
Causes of Keratoconus
There are no particular causes associated with keratoconus.
Genetic
Most of the children are born with keratoconus, and their condition worsens if proper care and treatment are not given to them. Studies have suggested that keratoconus is rather a hereditary disease than a normal occurring disease as keratoconus is known to run in families.
It is seen that the people with keratoconus condition have both the eyes affected and feel more comfortable in using eyeglasses to correct their blurry vision. There have been other studies that suggested that keratoconus is associated with other genetic disorders like down syndrome, osteogenesis imperfecta, and retinitis pigmentosa.
Natural Causes
There has been no evidence of any prior injury or any eye condition that would lead to a change in the shape of the cornea. It is observed that the shape of the cornea starts to change itself as early as in the teen years or as late as in the age of 30 and above. It has been observed that the change in the shape of the cornea is slow and takes several years. This change in the cornea can stop by itself or would continue to change itself for a period of several years. In some individuals, the change in the shape of the cornea is also caused due to the over-exposure to ultra-violet rays and due to chronic eye conditions.
The tissues present in the eyes can also break down due to various other factors including inflammation in the eyes due to allergy or atopic eye condition. The change in the vision caused by keratoconus occurs in two ways which are irregular astigmatism and an increase in near-sightedness of the person.
Irregular Astigmatism
The cornea in normal condition is usually dome-shaped and has a smooth surface, if a person gets affected by keratoconus then this shape changes to cone shape and the smooth surface becomes irregular or wavy in nature. This type of structure of the cornea causes irregular astigmatism. In some people, the front of the cornea expands to the extent that only objects placed near the eyes are visible and the distant objects are blurred. This type of keratoconus causes an increase in the near-sightedness of the person.
Rubbing of Eyes
The vigorous rubbing of eyes is also linked to an increase in the progression rate of keratoconus. Rubbing of eyes hard causes the breakdown of the cornea which in turn leads to faster progression of the eye condition.
Hormonal Imbalance
There also has been a study that suggests that due to hormonal imbalance the cornea becomes more susceptible to oxidative damage from the free radicals and leads to weakening and forward bulge of the cornea causes keratoconus.
Symptoms of Keratoconus
Getting a comprehensive eye exam can help ophthalmologists to determine keratoconus and can provide a better treatment option. Symptoms that may help you to determine whether you may suffer from keratoconus or not are having a double vision when looking with one eye open and the other eye closed, objects placed near and far appear blurry and only objects placed close to the eye are visible clearly, the appearance of halos around the bright lights, triple ghost images and appearance of light streaks, frequent need for a change of eyeglasses, clouding of vision, the appearance of scar tissue on the cornea due to its swelling and discomfort in the fitting of the eye lenses.
The other symptoms include a decrease in visual acuity, poor vision which can’t be altered using eyeglasses, impairment of visual perception, decrease in contrast sensitivity, photophobia ( sensitivity to light), eye strain, and irritation. Some symptoms like ghost images and decreased contrast sensitivity can also be seen in some other disorders including sclerotic cataracts.
Diagnosis of Keratoconus
Eye Exam
Diagnosis of keratoconus is made through an eye exam in which an ophthalmologist will measure the curvature of the cornea and will compare it with the normal cornea. Change in the measurement will suggest that there has been a significant change in the shape of the cornea. Mapping the surface of the cornea can also help in studying its surface and the detailed image can provide a current condition of the surface of the cornea.
Advanced Techniques
Advanced techniques like refraction, keratometry, corneal topography, and slit-lamp examination helps to diagnose keratoconus. Refraction of light caused due to cornea helps in diagnosing keratoconus. Patients who have keratoconus have blurry vision, myopia, and irregular astigmatism. Correction of vision is difficult to obtain in such cases as there is a continuous need for a change of contact lenses and eyeglasses. Corneal topography is used when biomicroscopy can’t determine the information related to keratoconus.
Treatment of Keratoconus
There are different shapes of the cornea like nipple cones, globes cones, and oval cones help in determining the shape of the cornea so that proper treatment can be provided according to your eye condition. Keratoconus is an eye condition in which the type of treatment depends on the severity of your condition. Your condition can be mild, moderate, or advanced, and depending upon it ophthalmologist will provide you with proper treatment.
- Mild Keratoconus
Mild keratoconus condition does not require any treatment as the vision is cured by wearing correct eyeglasses and contact lenses. Eyeglasses and contact lenses correct the distorted vision but as the shape of the cornea changes, the need to change the lenses is there to have a clear vision.
- Advanced Condition
Hard contact lenses are the lenses that fit the cornea correctly and are very rigid. They are generally used for advanced conditions in the keratoconus. These lenses may be uncomfortable at first and can adjust later on. Other alternatives of rigid lenses are the piggyback lenses which have a hard exterior and a soft interior. These are less uncomfortable and should be worn under proper prescription.
- Scleral Lenses
Scleral lenses are the lenses that sit on the sclera part of the eye rather than the cornea. They adjust themselves according to the shape of the cornea and are used in the advanced keratoconus condition in which the shape of the cornea changes fast.

- Prosthetic Lenses
They are the lenses that use advanced technology and relief the patients who have extreme discomfort in wearing the contact lenses. Prosthetic lenses are special customized lenses and are unique for each individual. They are made using special technology and provide a high-quality fitting to the cornea.
- Corneal Collagen Cross-Linking
Corneal collagen cross-linking is the therapeutic technique in which the cornea of the eye is stiffened to prevent further change in its shape. The cornea is first saturated with the riboflavin drops and then treated with UV rays. There are two types of corneal crosslinking which include epithelium on and epithelium off. In the epithelium off method, the upper layer of the cornea is removed in order to let riboflavin drops penetrate the cornea with ease.
In the epithelium on technique, the epithelium is not removed and riboflavin drops are directly put over them. The drops take time to penetrate the layers of the cornea. This method usually causes less discomfort and also a risk of getting any kind of infection through the epithelium on technique.
The cross-linking technique reduces progressive vision loss and stabilizes the cornea at the early stages of the disease. It also reduces the possible chances of getting a corneal transplant.
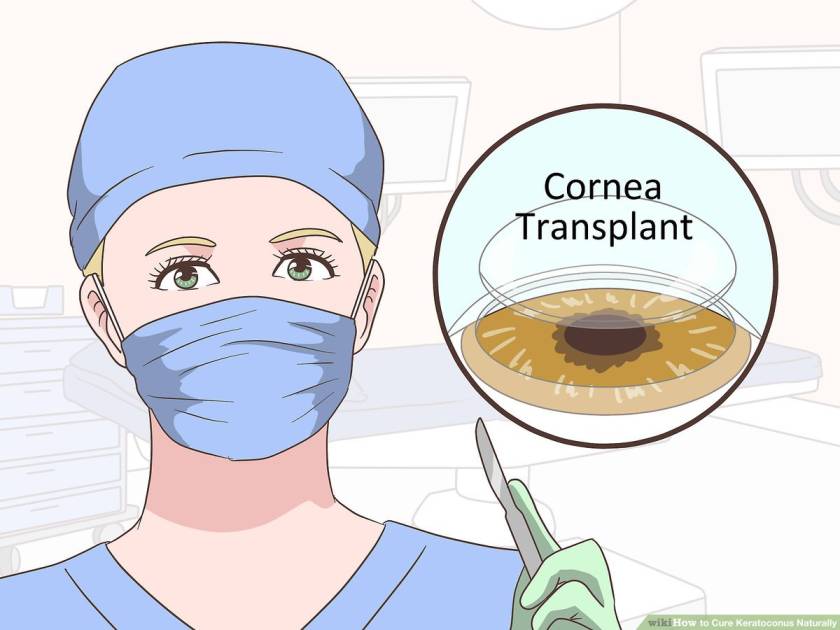
- Surgery
The surgical option includes the removal of the cornea and replacing it with the new cornea. This is called penetrating keratoplasty and the whole cornea is replaced in this surgical process. The other surgical option includes deep anterior lamellar keratoplasty in which only the outer lining of the cornea is replaced with the donor’s cornea and the inner lining is not replaced. This type of surgery avoids the rejection of the donor’s cornea by the immune system of the person.
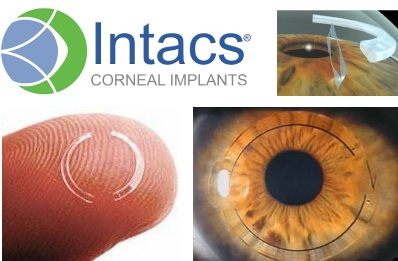
- Intacs
Intacs are medical devices that are used to treat keratoconus. In this, the Intacs are inserted in the cornea and they then reshape the cornea into a flatter and dome shape. The vision of the person receiving this treatment is restored to a certain level and eyeglasses and contact lenses can be used by them after the treatment.
- Conductive Keratoplasty
Topographic guided conductive keratoplasty is a handheld machine that is used to reshape the cornea back to its normal dome shape using the radio waves generated by the machine. Irregular astigmatism which is caused due to keratoconus can be easily treated by this method.
- The Best Option For You
Surgical options are best suited for those people who have advanced stages of keratoconus. Mild conditions can be handled by wearing eyeglasses and contact lenses to clear the vision. Reducing corneal sensitivity and tear secretions and the use of rigid contact lenses help in easing mild conditions of keratoconus. Surgical options are used when contact lenses are not helpful in providing a clear vision which may occur due to inadequate acuity, peripheral thinning, and inadequate lens tolerance.
Prevention of Keratoconus
Prevention of keratoconus can be done by protecting eyes from UV rays, wearing properly fitted contact lenses, and not rubbing your eyes. Keratoconus can’t be completely prevented but can slow down its progression. It is advised to visit a doctor for a proper consultation and to get the best treatment according to your condition of keratoconus. A proper eye exam can help in the early detection of keratoconus which will be helpful in slowing down the progression of the disease.



