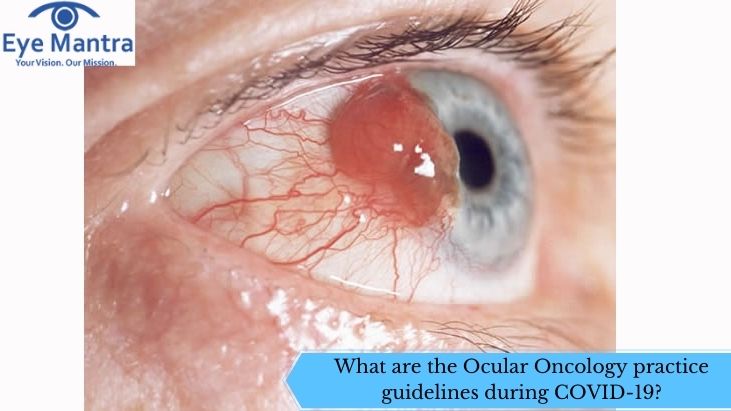
The pandemic has caused many changes in the healthcare industry, it also resulted in a temporary suspension of oncology services due to a delay in diagnosis and treatment. Therefore, in order to continue the ocular oncology treatment, a set of new guidelines are formed. Ocular oncology is a branch of medicine that deals with various tumors of the eye which includes eyelids, eye orbit, intraocular structures, and ocular surface.
In 2020, the coronavirus pandemic created a major problem as many patients suffering from ocular oncology conditions and other cancer patients could not be treated effectively. Due to this, in May 2020, a group of a multidisciplinary team including various ophthalmologists, ocular oncologists, medical oncologists, radiation oncologists formed a report which consists of various guidelines. It helped in running the ocular oncology service even in this pandemic situation. Moreover, it helped to strike a balance between the treatment of patients as well as to provide them protection from the COVID-19 pandemic. Some of the guidelines reported are:
Screening and triage of patients
In this, the guidelines for the basic screening as well as the triage of patients are covered. The triage of patients is done at four levels- quad triage which consists of online registration, online or teleconsultation of specialists or doctors to the patient, physical screening, and later clinical evaluation that helps in determining the severity of the problem in the patient.
Online tests help in decreasing the risk of the spread of coronavirus. A patient who is suspected to be suffering from the corona is shortlisted and as per the guidelines given by the Ministry of health and family welfare is sent for corona testing and treatment is done when the patient is proved negative.
But, if the patient is shown as positive, then the patient is sent directly to the investigation, and the rest of the treatment is done at the government-designated COVID-19 centers. In case of an emergency such as the presence of unbearable pain or inflammation near the eye, nausea, or risk of loss of vision, then the patient is given treatment in a pre-designated spot along with a specialist who is given full personal protection equipment (PPE) for his safety and primary treatment that can help in reducing the symptoms is given to the patient before sending him or her to the COVID-19 care center. In a case of bearable symptoms in the treatment of ocular oncology, then the treatment is delayed until the patient is given treatment for COVID-19.
Safety of healthcare workers
The safety of healthcare workers i.e, doctors and nurses who treat patients is of top priority as they can provide help to most of the patients suffering and are considered as a valuable resource for any country in the world. Proper handwashing and use of antiseptics, as well as the use of masks and covers for proper protection of the patients, must be enforced. The use of personal protective equipment (PPE) is enabled for the safety of doctors is classified into two:-
- Full personal protective equipment
- Essential personal protective equipment
Safety measures for surgical procedures used in ocular oncology
During ocular oncology conditions, surgery is also performed for treating ocular oncology. Generally, the risk of virus transmission is majorly carried out by aerosol-generating procedures (AGP’s) which include procedures such as intubation, extubation, high flow of nasal oxygen, open suctioning of the respiratory system. In this case, the use of local anesthesia is preferred over the use of general anesthesia.
Guidelines for specific diseases in ocular oncology:
- Retinoblastoma: In this disease of ocular oncology, there is an examination under anesthesia, also called EUA. In EUA, there is a greater risk of transmission of the virus. Hence during this ocular oncology treatment, the patient, as well as the doctor, is completely covered using personal protective equipment which consists of long sleeves, protective eyewear, protective gloves, and a mask that covers the nasal part along with the complete facial part decreases the risk of virus transmission.
A virucidal fluid i.e, 5% Povidone-iodine solution is given to the conjunctival sac inside the eye before performing the ocular oncology surgery. Disinfection of the lens, as well as the indirect ophthalmoscope, must be done after every examination of the ocular oncology condition.
- Uveal melanoma: This is a newly diagnosed disease of the ocular oncology condition which is treated instantly because of its dangerous nature. Evaluation of this disease is done with the help of an indirect ophthalmoscope along with the use of ultrasonography documentation.
The surgical treatment is done by the use of general anesthesia (GA). With the help of retina specialists or ocular oncologists, the surgery must be performed under the guidelines of COVID-19 care. After the ocular oncology treatment, the use of anti-VEGF injections as follows up after radiation therapy can be delayed for one or two months used for retinopathy.
- Benign intraocular oncology: In this case, the decrease of vision is due to extubation as well as fluid accumulation in the sub-foveal region. This type of tumor is diagnosed by the fundus fluorescein angiography (FFA) procedure. The delay of the treatment for this disease is not preferable as there is a risk of loss of vision. Laser therapy must be performed as per the existing protocols or norms.
- Orbital tumors of ocular oncology: These tumors need an immediate response i.e, immediate treatment as they can cause permanent loss of vision, death, or visual disability. Exposure to sinus mucosa during the surgery can cause a higher risk of virus transmission. In this case, care must be taken so that there is no breach into the orbital wall inside the eye.
- Eyelid tumors of ocular oncology: Many eyelid tumors which are some lethal ones such as sebaceous gland carcinoma, Merkel cell carcinoma require proper treatment along with care. Other eyelid tumors such as basal cell or squamous cell carcinoma cannot be delayed and need immediate treatment as it can cause loss of complete vision of the eye.
The laboratory pathologist must be informed prior to the surgery so that the laboratory can be prepared on time and the staff must be provided with safety measures such as protective gloves, protective glasses along with full personal protective equipment so that the disease transmission is reduced. However, the post-operative check-up for ocular oncology is performed as per the existing protocols.
Pathology guidelines of ocular oncology
As this COVID-19 pandemic is a risk of disease transmission from patient to the ocular oncologists. Hence, the following protocols must be followed for the protection from the coronavirus in ocular oncology treatment. The protocols are:
- Perfect cleaning of the laboratory with utmost care is done.
- The use of N95 masks along with protective eyewear, protective gloves is a must.
- The specimens must be enclosed in well-fitted containers during their transplantation to avoid leakage.
- The frozen section of the unfixed tissues has a greater risk of virus transmission. The specimens of ocular oncology parts that are under a huge risk of virus transmission are conjunctiva, nasal, and sinus specimens.
- During fixation, the tissues must be kept moist. During fixation, tissues must be kept for about 24-48 hours.
- Use of 1% sodium hypochlorite is done for disinfection of working areas and cleaning of instruments used.
The patients undergoing COVID-19 treatment must be placed in isolation, separate from the other patients and proper hand washing and taking proper care helps in improving the immune system of the ocular oncology patients.
The best way to treat your eyes is to visit your eye care professional and get your eyes checked regularly. He will be able to assess the best method of treatment for your eye ailment. Visit our website Eyemantra.To book an appointment call +91-9711115191. Or mail us at [email protected].Our other services include Retina Surgery, Specs Removal, Cataract Surgery, and many more.